When President Obama signed the Affordable Care Act in 2010, there was the hope for health care equality for all. Along with this reform, the goal of better access to health care that was of higher quality and that was affordable for individuals, families, businesses and taxpayers was central. The most recent statistics show that in 2014, more Americans had access to preventative and diagnostic health care than at any point in our nation’s history.
 With $17.2 trillion dollars in annual spending, the United States has the richest economy in the world. Health care spending in 2013 was estimated at $2.9 trillion dollars or an average of $9,225 per person, according to statistics provided by CMS. The amount spent on health care has increased at least 3.6% per year for the past five years.
With $17.2 trillion dollars in annual spending, the United States has the richest economy in the world. Health care spending in 2013 was estimated at $2.9 trillion dollars or an average of $9,225 per person, according to statistics provided by CMS. The amount spent on health care has increased at least 3.6% per year for the past five years.
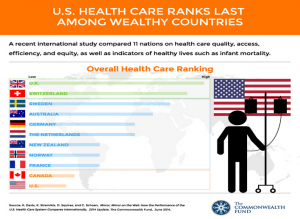
But, does spending a lot on health care equate to good health outcomes? According to a study conducted by the Commonwealth Fund, the United States continues to rank poorly on indicators of healthy lives, such as mortality amenable to health care, infant mortality, and healthy life expectancy at age 60. To be blunt, Americans die younger and experience more injury and illness despite spending nearly twice as much on health care in comparison to other wealthy countries.
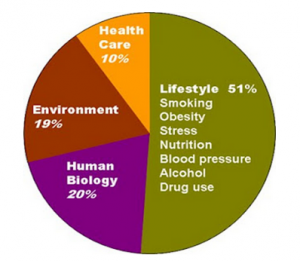
It’s very clear that achieving good health requires much more than spending money on health care. We have more people with insurance, which leads to more people seeing a primary care physician, but are we following the recommendations our doctor is giving us?
What we eat, how much physical activity we participate in, how we manage stress, and our use or misuse of alcohol and drugs has a significant impact on health, even more so than access to health care. As much as the industry tries to develop a magic pill to give us good health, the primary challenge is the lifestyle choices we as individuals make on a day to day basis.
If we do a timeline comparison of expensive medical advancements, along with modern conveniences including how we move about (automobiles, elevators, airplanes), our sedentary entertainment and communication channels (televisions, computers, and smartphones) and what we eat (fast food, packaged meals, junk food), we create a perfect storm of high cost care and poor health outcomes.
In the United States, the biggest threat to good health is obesity. In Michigan, the obesity rate is estimated to be 31.5%, according to the CDC, with 66% of the adult population considered to be overweight. These challenges are not just with adults, as we see an epidemic of childhood obesity. Back in 1970, the childhood obesity rate was 5%. In 2010, it was 17%. In Michigan, almost 27% of adolescents were overweight or obese. The primary precipitators were too little physical activity, too much TV and computer usage, and too few fruits and vegetables as part of a regular diet.
Given our current health status, what we are seeing as a first step to good health is a change in public policy to impact health outcomes. The early data shows some success with programs like Michelle Obama’s “Let’s Move” program, the ACA’s & FDA’s requirements on labeling all foods with nutritional information, including menus at restaurants with 20 or more chains, the Healthy, Hunger Free Kids Act that determines nutritional value of school lunches, and new Health and Behavior Intervention (HABI) codes allowed by Medicare and some commercial insurances to cover behavioral health interventions to treat medical conditions.
Companies have a renewed focus on improving employee health and wellness. More parks are being built or refurbished every year, and many include walking trails and organized recreational activities at low or no cost. As evidenced by the furor over the attempted ban on super-sized soft drinks in New York, we tend to resist governmental interference with our right to create our own poor health outcomes. Clearly, the choice to be healthy or unhealthy is an inalienable right.
The second step to good health is increased attention to self-management of good health. Patient-Centered Medical Homes, Health Homes, and outcomes-based payment have led to a greater level of responsibility on the part of the primary care or behavioral health provider to provide wellness education and treatment services to patients. The continuous review of health status and the development of a wellness plan will soon be standard clinical practice. The availability of counseling services for people needing support in working on wellness, as well as coverage for this service, is conditional on how invested the clinic is in wellness.
The third step to good health is creating healthy habits that enhance health. There is no magic pill that will cure obesity, or take the place of living a healthy lifestyle. It’s a simple formula containing the following:





The primary thing we need to understand is that access to health care is just one piece of good health. A doctor can diagnose and treat conditions but making simple changes every day can lead to better health.

Kathy is a consultant and trainer with the National Council for Behavioral Health, providing integrated care consultation and case to care management training sessions across the United States. Kathy holds a Master’s degree in counseling psychology and has worked in the community mental health field for over 26 years.
Phone: (517) 712-5593 | Email: kdettling@afiahealth.com | LinkedIn