
Electronic Health Records are a failure. They lower productivity. They decrease provider satisfaction. They don’t increase clinical quality. They haven’t lived up to their promises.
These are statements that I hear more and more frequently as healthcare organizations across the country adopt EHRs. Working closely with these organizations for the past decade I’ve seen firsthand the issues that staff experience, and lately I’ve begun asking myself, are they right?
I think the issue is much more complicated, though. First of all, our expectations for technology in the digital age are so high that if something doesn’t do the work for us, we think it’s a waste. It is a world of instant technological gratification. Google can provide us information on any topic that we can think of, anywhere we are, any time we want it. We can watch television on-demand on our phones. We can use an app to scan the barcode of almost any product at any store to instantly see if the price is competitive and to get reviews on the item from other shoppers all over the world. When these are the types of technologies that have come to define our baseline expectations for user experience, we can begin to understand why the bar is set so high for EHRs.
Another significant issue that has caused dissatisfaction with EHRs has to do with the way in which the implementation approach. Most organizations don’t realize the level of effort, and the steps, that it takes to implement an EHR properly. Following the plan from the vendor, and getting a system live, is only half of the battle. Without the proper workflow analysis and internal dialogue, an EHR will never be optimized to support the clinical, financial, and administrative components of a large healthcare organization. And considering that the EHR vendors have been under water for a decade just trying to keep up with the demand for their systems, driven by financing and regulatory reforms, they’ve had no time to adjust their processes to help support this effort.
So, why can’t we just “uberize” the EHR experience and be done with it? I think there are three reasons why this hasn’t happened in the past, and likely won’t happen for years to come.
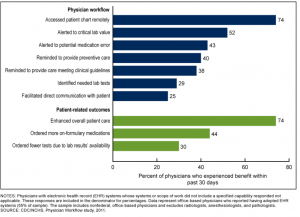
Now, with all of that said, we do have to look at the flip side of this coin. While Electronic Health Records may not achieve all of the promises made a decade ago, there have been substantial benefits to the electronic age of healthcare. A few of those include:
So while Electronic Health Records may not necessarily have lived up to their original hype, there are significant benefits to their adoption for providers, clients, and the healthcare system as a whole if they are implemented and adopted properly. There are also incredible opportunities to begin building off the foundation that EHRs are creating. The data that providers have been capturing in their EHRs should be used to educate organizations on the changes they need to make to provide better care, maintain healthy margins, develop new services and programs, and excel in the world of value-based payments. This may just be the real promise of EHRs, and it makes it an exciting time to be working in the world of healthcare technology.

Author Matt Hoffman is a Managing Partner at Afia (afiahealth.com). During his time as a healthcare consultant, he has worked with dozens of healthcare organizations to transform them into more effective and efficient care providers.
Phone: (734) 249-8402 | Email: matt@afiahealth.com | LinkedIn
* Reduction in medication errors in hospitals due to the adoption of computerized provider order entry systems. Radley DC, Wasserman MR, Olsho LE, Shoemaker SJ, Spranca MD, Bradshaw B.
** Jamoom E, Beatty P, Bercovitz A, et al. (2012) Physician adoption of electronic health record systems: United States, 2011. NCHS data brief, no 98. Hyattsville, MD: National Center for Health Statistics.